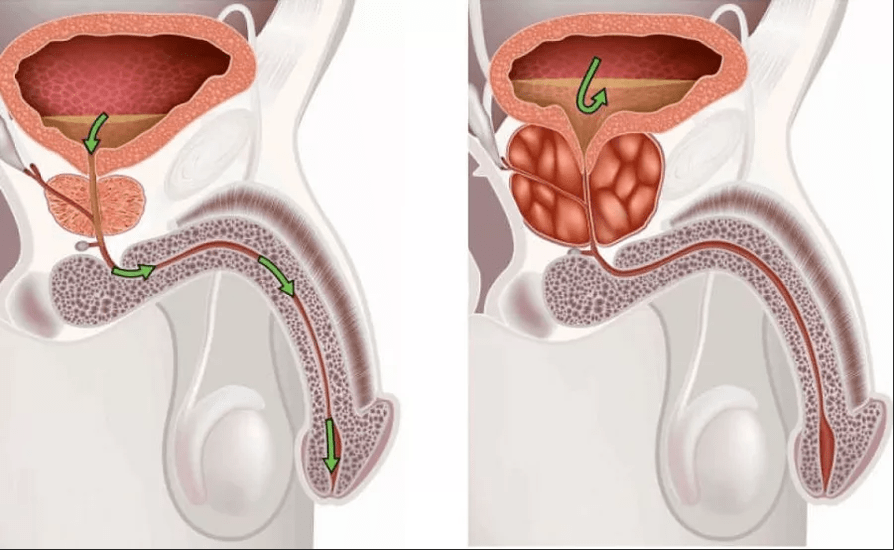
Prostatitis is an inflammation of a person's prostatic gland.The prostate is located just below the bladder and the size of a chestnut.He surrounds the first section of the urethra and extends to the SO-appeal pelvic floor, which consists of muscles.

Prostate produces secretion, which includes PSA and semen.The PSA makes the ejaculate more liquid.Spermine is important for the mobility of sperm.
Prostatitis is mainly associated with intense pain in the perineum and the anal region.In addition, symptoms such as the frequency of urination, pain during urination and pain during ejaculation occur during the inflammation of the prostate.
The prostate is relatively often affected by inflammation.The probability of prostate infection increases with age.Studies show that most cases aged 40 to 50.
Prostatitis syndrome
At the same time, an extended understanding of the term prostatitis appeared in medicine.With SOP prostatitis syndrome, several complaints are summarized in the human basin area, which generally have an unknown reason.The term "prostatitis syndrome" sums up various clinical paintings:
- Acute bacterial prostatitis
- Chronic bacterial prostatitis
- Inflammatory and non -inflammatory syndrome of chronic pelvic pain
- Asymptomatic prostatitis
Acute and chronic bacterial prostatitis
Acute prostatitis is caused by bacteria.The bacteria cross the blood to the prostate, either propagate from the bacterial infection of the bladder or the urethra with the prostate.Acute prostatitis is generally a serious general condition with intense pain during urination, fever and chills.
Chronic prostatitis can develop from Acute: if for more than three months, there is inflammation of the prostate gland and repeated microbes in urine, expression of prostate or ejaculate, then it is chronic inflammation.
Bacterial prostatitis.It is less lightning speed than acute prostatitis.Although the chronic inflammation of the prostate gland causes pain during urination and, possibly, a feeling of pressure in the perineum, but complaints are generally not as expressed as in acute prostatitis.
Chronic pelvic pain syndrome (abacterial prostatitis)
In most cases, prostate infections, bacteria cannot be detected in urine, prostate or ejaculate as the cause of the disease.The trigger for prostatitis remains uncertain.Doctors call it chronic pelvic pain.
However, in such cases, leukocytes can often be detected as an expression of inflammation in the prostate gland.To differentiate this, another form of the disease in which neither bacteria nor leukocytes are detected.Chronic pelvic pain syndrome is the most common form of prostatitis.
Asymptomatic prostatitis
In rare cases, asymptomatic prostatitis occurs.With this form of prostatitis, although there are signs of inflammation, but there is no pain or other symptoms.Asymptomatic prostatitis is generally detected by accident, for example, as part of a study of infertility.
Prostatitis: symptoms
Prostate inflammation can cause various symptoms of prostatitis.Although symptoms of acute prostatitis can be very serious and cause a strong feeling of discomfort, with chronic prostatitis, they are generally a little lower.
Acute prostatitis: symptoms
Acute prostatitis is often an acute disease in which patients suffer from fever and chills.The urination causes burning pain and the flow of urine is significantly reduced due to the edema of the prostate gland.Since the victims can only distinguish a small amount of urine, they have a frequency of constant urination and must often go to the toilet.Other prostatitis symptoms include bladder, pelvic pain and back pain.Pain can also occur during or after ejaculation.
Chronic prostatitis: symptoms
Prostatitis with a chronic course generally causes symptoms less serious than acute inflammation of prostate.Symptoms such as fever and chills are usually completely absent.Symptoms, such as a feeling of pressure in the perineum or the lower abdomen, the darkening of ejaculate due to blood in sperm or blood in the urine is typical of the chronic inflammation of the prostate. Symptoms of chronic and chronic abacterial bacterial prostatitis do not differ.
Prostatitic complications
The most common complication is the abscess of the prostate.The abscess of the prostate gland is a purulent inflammation of inflammation, which must generally be open and empty with a cut.
To complicate more the inflammation of the prostate, inflammation can apply to neighboring structures, such as the appendix of the testicle or testicles.It is also suspected that chronic prostatitis is associated with the development of prostate cancer.
Prostatitis: causes and risk factors
Bacterial prostatitis: causes
Only ten percent of prostatitis are caused by a prostate bacteria.Bacteria can enter the prostate by blood or neighboring organs, such as bladder or urethra, where they can cause an inflammatory reaction.
The bacteria of Escherichia coli, which is mainly in the human intestine, is the most common cause of prostatitis.Klebsiella, Enterococci or Mycobacteria can also cause prostatitis.Bacterial prostatitis can also be caused by sexually transmitted diseases such as chlamydial or trichomonas infections, as well as by Gonorrhea.
In chronic prostatitis, bacteria of the prostate gland have avoided the not yet clarified way of protecting the human immune system.This allows microbes to constantly colonize the prostate.Antibiotics are relatively poor in the fabric of the prostate gland, which can be another cause of bacteria survival in the prostate gland.
Chronic pelvic pain syndrome: Causes
The exact causes of chronic pelvic pain syndrome have not yet been fully studied.Scientists have appointed many theories, each which seems plausible, but all have not yet been clearly proven.In some cases, the genetic equipment of previously unknown microorganisms was found in the basin.Therefore, the cause of pelvic pain syndrome can be microorganisms that still cannot be cultivated in the laboratory and, therefore, are not detected.
Another possible cause of chronic pelvic pain is bladder disorders.Due to altered drainage, the volume of the bladder increases, which thus presses the prostate.This pressure ultimately damages the fabric of the prostate gland, causing inflammation.
However, in many cases, the cause of chronic pelvic pain cannot be clearly demonstrated.Then doctors talk about idiopathic prostatitis.
Anatomical causes
In rare cases, prostatitis is caused by the narrowing of the urinary tract.If the urinary tract is narrowed, the urine accumulates and, if it enters the prostate, it can also cause inflammation.This narrowing can be caused by tumors or the prostate stones if called.
Mental reasons
Recently, more and more psychological causes of prostatitis have been discussed.In particular, with a non -inflammatory syndrome of chronic pelvic pain, a mental trigger is likely.The exact mechanisms are still unknown.
Risk factors for prostatitic development
Some men are particularly at risk of developing prostate infection.These include, for example, men with a violation of the immune system or removed by the immune system.In addition, the main diseases, such as diabetes mellitus, can contribute to the development of prostatitis: increased blood sugar in diabetes patients often leads to an increased level of sugar in the urine.The abundant sugar content in urine can provide bacteria with good growth conditions, facilitating the development of urinary tract infections.
Another risk factor in the development of prostatitis is the coatter of the bladder.The introduction of a catheter through the urethra through the urethra can cause small ruptures of the urethra and damage to the prostate gland.In addition, as on any foreign body, bacteria can settle on the bladder and form the biofilm if called.As a result, bacteria can increase along the urethra to the bladder, as well as lead to prostate infection.
Prostatitis: exams and diagnostics
A general practitioner can take medical history, but if there is a suspicion of prostatitis, he will head to a urologist.This performs a physical exam.In the event of suspicion of prostatitis, it is generally the digital rectal study if called.Nevertheless, this study does not give clear proof of the inflammation of the prostate, but only confirms suspicion.To detect bacterial prostatitis, a laboratory examination can be carried out
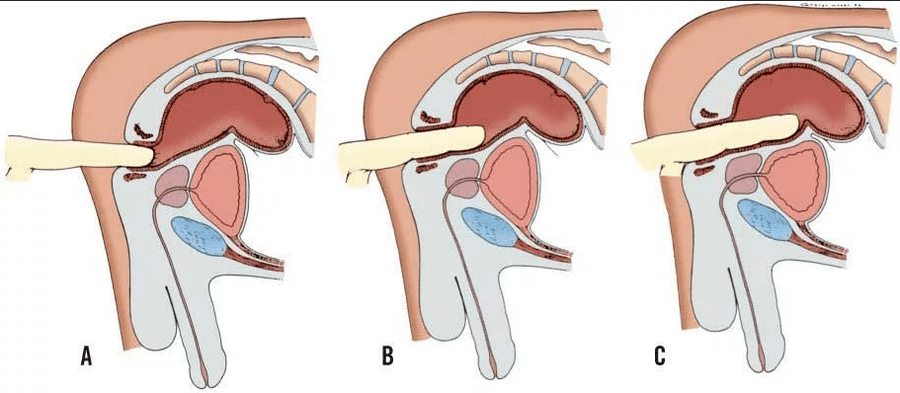
Rectal examination of the fingers
Since the prostate gland borders directly with the rectum, it can be palpated in the rectum.This digital rectal study is carried out on an outpatient and without anesthesia, generally without pain.The patient is invited to lie down with folded legs.Using a lubricant, the doctor then slowly inserts the finger into the anus and scored the prostate and the adjacent organs.It examines the size and sensitivity to pain in the prostate gland.
Laboratory
To identify the pathogens possible in most cases, an urine analysis is carried out.The standard method is the sample thus called four glasses.Here, Erturin, Mittelsstrahlurin, Prostataexprimate and Urine are tested after massage of the prostate.As prostaxprimate called it, doctors call the secretion of the prostate.This is carried out by a doctor by a slight pressure on the prostate, for example, on palpation.Ejaculate can also be tested for pathogenic microorganisms and signs of inflammation.
Additional research
The ultrasound of the rectum can be used to determine exactly where the inflammation is and how far it has spread.An important objective of the study is also the exclusion of other diseases with similar symptoms.
To exclude that the existing violation of urine drainage is caused by the narrowing of the urethra, the urinary flow is measured.The normal flow of urine is 15 to 50 milliliters per second, while the flow of urine is ten milliliters per second or less, there is a high probability of obstruction of the urethra.
Prostatitis: treatment
Pharmacotherapy
Acute bacterial prostatitis is treated with antibiotics.In soft cases, the dose of the antibiotic is sufficient for about ten days.In chronic prostatitis, the drug must be taken for a longer period.According to pathogenic microorganisms, active substances of luxacin, ciprofloxacin, azithromycin, erythromycin or doxycycline are appropriate.Even if the symptoms are already thinning, antibiotics must in any case continue in accordance with the appointment of a doctor.
In addition, asymptomatic prostatitis is treated with antibiotics.
If there is chronic abacterial prostatitis, antibacterial therapy is generally ineffective.With inflammatory chronic pelvic pain syndrome, despite the lack of evidence of the presence of a pathogen, a study is carried out using antibiotics, because sometimes an improvement can be carried out.However, with non -inflammatory chronic pelvic pain syndrome, antibiotic therapy is not recommended.
Other therapeutic approaches to chronic abacterial prostatitis are the so-called 5α-reward inhibitors, such as deride or dutasteride, pentosan polyisulfate and plant drugs, such as quercetin or dust extract.If the improvement is not obtained, the drug treatment will be supplemented in physiotherapy.Here, physiotherapy exercises, exercises for the pelvic floor muscles or a regular prostate massage are recommended.
In addition, symptomatic treatment can help relieve the acute symptoms of prostate infection.Anesthetics can be prescribed for intense pain.In addition, heating pads and heating pads at the rear or at the bottom of the abdomen help to relax the muscles.This often relieves pain with the inflammation of the prostate.
Relapse
The frequency of relapse of prostatitis is generally very high.About 23% of victims are subject to the second episode of the disease after an illness, 14% suffer from three and 20% - even from four or more cases.To reduce the risk of relapse, avoid wearing wet clothes during or after prostatitis, hypothermia or use of bubbles, such as black tea or coffee.This reduces the risk of cystitis and, therefore, prostatitis.However, you cannot reliably prevent bacterial prostatitis using these methods.
The prognosis of prostatitis depends, on the one hand, on the cause of inflammation and on the other, the speed with which correct therapy begins.
In acute bacterial prostatitis, which is treated as soon as possible with antibiotic therapy, the prognosis is generally good.Taking antibiotics, pathogens die, which generally prevents transition to chronic prostatitis.
About 60% of all patients with acute prostatitis have no more symptoms in six months and around 20% develop chronic prostatitis.Treatment and prognosis are more difficult here.In many cases, periodic episodes of the disease can accompany those who suffer for many years.
Chronic prostatitis generally requires great patience of the victims.Very often, a long course can be a serious psychological burden.
Patients who have suffered should request professional help because the mental health situation has a huge impact on prostatitis forecasts.






















